In October 2017, I developed deep vein thrombosis (DVT) and pulmonary embolism (PE) in both lungs. To mark World Thrombosis Day—observed annually on October 13—I share my experience of these life-threatening conditions.
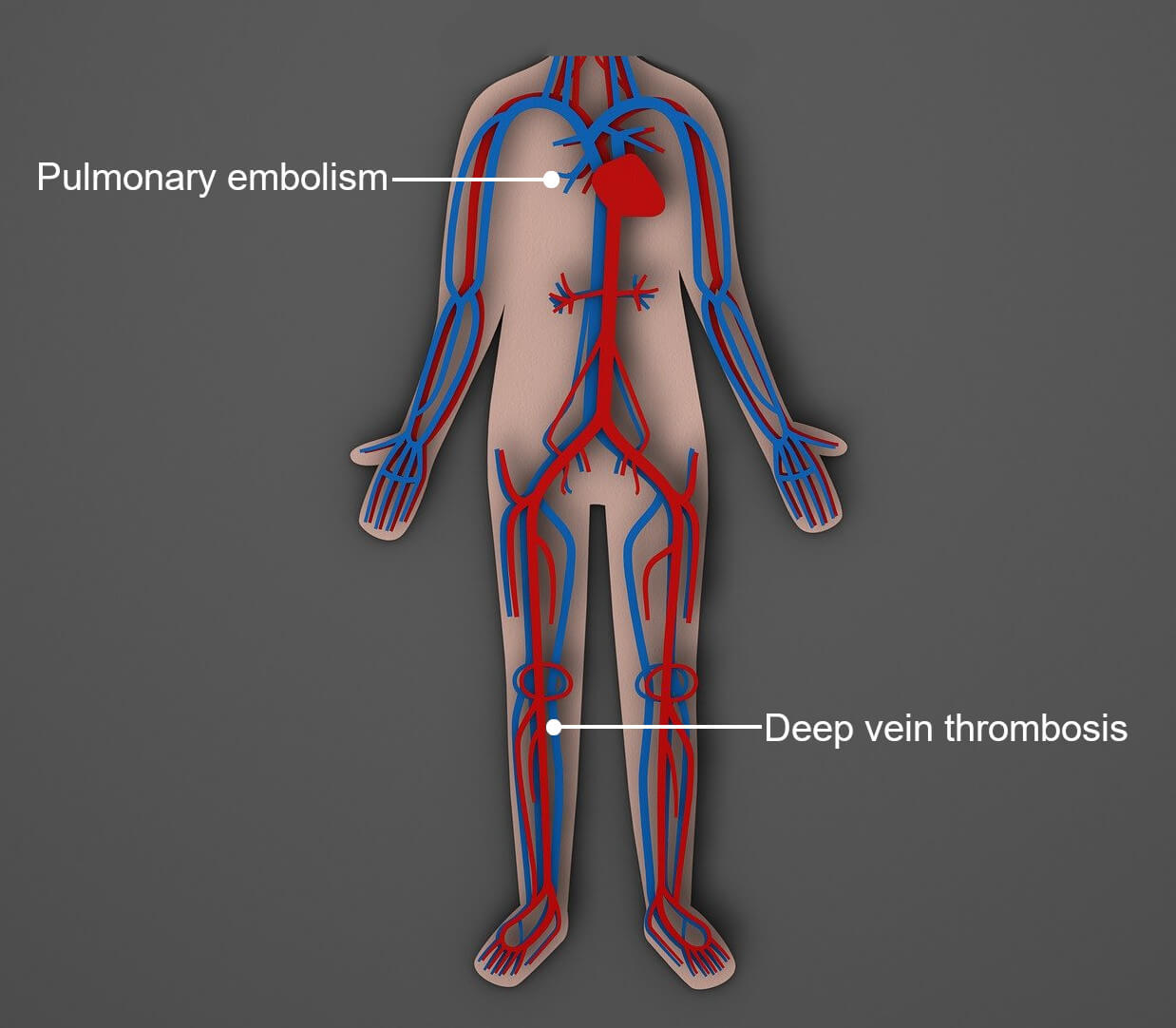
Signs and symptoms of DVT are often misleading or nonexistent. But left untreated, the condition can lead to PE—a life-threatening complication.
If you’re experiencing mysterious or unexplained aches and pains in your leg or foot, make sure your doctor examines you for DVT. Apart from saving you a lot of trouble, it could save your life.
In this post, I recount my own experience of DVT and PE, drawing particular attention to how confusing symptoms can be and why you might need to question your doctor’s opinion. I also share insights into causes, symptoms, treatment, and preventive measures.
What Is DVT?
DVT is a clot (or thrombus) within a large vessel of the deep vein system. It typically forms in the lower leg, thigh, or pelvis, but may occur in the arms, kidneys, intestine, liver, or brain.
How Clots Form
In response to vessel injury, clotting factors consisting of fibrin (a protein) and platelets (a type of blood cell) clump together at the site of the wound to form a clot, which acts as a plug to stop the bleeding.
DVT occurs when a clot forms within an intact vessel.
What Causes DVT?
Lack of Activity
Lack of activity is the most well-known cause of DVT. When we are inactive, circulation slows, causing blood to pool in the lower extremities. This is a usual daily occurrence, with normal blood flow resuming the moment we begin to move again.
But over extended periods, there’s an increased risk of clots forming in the pooled blood. Situations where this may occur include surgical operations lasting more than 60 to 90 minutes, being on bed rest for more than three days, wearing a cast, and car journeys or flights of more than four hours.
Because DVT often occurs during or after long-haul flights, it’s sometimes referred to as “economy class syndrome.”
Damaged Blood Vessels
If a vessel narrows or becomes blocked due to damage, restricted blood flow may cause a clot. Such damage can occur through surgery of the legs, hips, pelvis, or abdomen, as well as broken bones and muscle injuries.
 Source: Pexels/Pixabay
Source: Pexels/PixabayWho Is at Greater Risk?
Lack of activity and damaged blood vessels can cause anyone to develop DVT, but certain medical conditions, lifestyle choices, and age can significantly increase the risk.
Cancer
Cancers of the pancreas, stomach, colon, and lungs, among others, release substances that raise the level of clotting factors. It’s therefore essential to carry out all age-appropriate screenings after a DVT diagnosis.
DVT can also be a side effect of certain cancer treatments.
Bowel Diseases
Insufficient fluid intake or loss of fluid leads to a thickening of the blood, which in turn facilitates clotting. Due to the dehydrating effect of diarrhea or problems absorbing fluids, people with gastrointestinal disorders (e.g., Crohn’s disease and ulcerative colitis) are at particular risk.
Other Risk Factors
Risk also increases if you are a smoker, obese, older than 40, have previously experienced DVT, and/or have a family history of DVT, which may indicate a genetic mutation affecting the clotting mechanism.
The Neat and Tidy Man focuses on men’s grooming and well-being. But here are risk factors exclusive to women for whatever reason they may be relevant to you:
- Pregnant women: Due to elevated estrogen levels, which raise the value of certain clotting factors, the risk of developing DVT increases throughout pregnancy and for up to six weeks thereafter.
- Women using hormone drugs: For the same reason, risk increases for women using the contraceptive pill or receiving hormone replacement therapy (HRT). But risk level depends on how the drug is administered; transdermal is considered safer than oral. Another consideration is whether the drug incorporates progestin; there’s no risk attached to the progestin-only pill, but women being treated with both estrogen and progestin are at greater risk than those being treated with estrogen only.
Symptoms of DVT
You may experience no symptoms at all, or one or more of the following:
- An ache or cramp-like pain that usually begins at the back of the calf. This may intensify when putting weight on it—for example, through standing and walking.
- Your leg, ankle, or foot may be swollen, warm to the touch, itchy, and/or turn red, blue, or purple.
- Veins near the skin’s surface may be tender to the touch and swollen.
What Is PE?
Pulmonary embolism occurs when part of a clot in another body region, usually a leg, breaks off and travels to the lungs.
When PE results from DVT, the condition is known as venous thromboembolism, or VTE.
The Difference Between Thrombosis and Embolism
A thrombus is a clot that remains at its point of origin. An embolus is something (anything) that travels through the bloodstream before lodging in a vessel that is too narrow for it to pass.
Symptoms of PE
You may experience no symptoms at all, or one or more of the following:
- Shortness of breath, often sudden.
- A sharp chest pain that worsens when coughing, inhaling, bending, or eating.
- A dry cough.
- Coughing up bloody sputum.
- Wheezing.
- Rapid breathing.
- Rapid or irregular heartbeat.
- Blue lips and/or nails.
- Low blood pressure.
- Sweating.
- Feeling lightheaded or faint.
- Anxiety.
Unless symptoms of DVT are also present, there’s a good chance that health professionals won’t associate these with PE.
An Account of My Symptoms
My initial symptoms differed from any of those listed above, which led to a delayed diagnosis.
- Sunday, September 17, 2017: At home working at the computer, I suddenly sensed something slip or move within my lower left leg. Afterward, it felt as though there were a huge, boil-like lump in the arch of my foot, which caused pain only when standing and walking. Internet research indicated that I may have developed plantar fasciitis, an inflammation of the ligament connecting the heel to the toes.
- Friday, September 22, 2017: The pain had worsened. The only way I could get about was by bicycle, using my toes to pedal. After running his hands over my leg and foot, an orthopedist advised that I wear a bandage and take a magnesium supplement. Although unable to make a diagnosis, he ruled out plantar fasciitis and DVT. I later learned that it’s impossible to detect DVT with the bare hands.
- Monday, September 25, 2017: Cycling to work, I had to keep stopping for breath, which meant gasping for air with what seemed like limited lung capacity. On reaching the office, I had a coughing fit so violent that I had to leave the room. I wondered if I was suffering the long-term effects of the 40-to-80-a-day cigarette habit I’d quit five years earlier. But over the next few days the symptoms passed, including the pain in my foot.
- Sunday, October 8, 2017: At home working at the computer, I again felt something move in my lower left leg. This time it left me with a cramp-like pain at the back of the calf.
- Monday, October 9, 2017: Similar pains developed in my right leg, and I was once again short of breath. Internet research indicated the possibility of PE resulting from DVT, but the orthopedist had ruled this out. A further possibility was chronic venous insufficiency resulting from varicose veins deep within the leg. As a precaution, I purchased a pair of compression socks.
- Tuesday, October 10, 2017: I informed my employer that I’d be visiting a doctor the following morning. The pain in my right leg had vanished, but risen to the thigh in the left, and I was still short of breath. Removing my compression socks that evening, I noticed that my left foot was slightly swollen and had turned purple. Suspecting DVT and PE, I took a cab to the nearest emergency room.
 Source: Mr Thinktank via flickr.com (CC BY 2.0)
Source: Mr Thinktank via flickr.com (CC BY 2.0)Diagnosis and Initial Treatment
After summarizing my symptoms, a doctor at the reception mockingly dismissed the notion that I might have developed DVT. If I had, she said, my foot would be warm to the touch and red, not purple. But on closer inspection, she realized immediately that it was DVT.
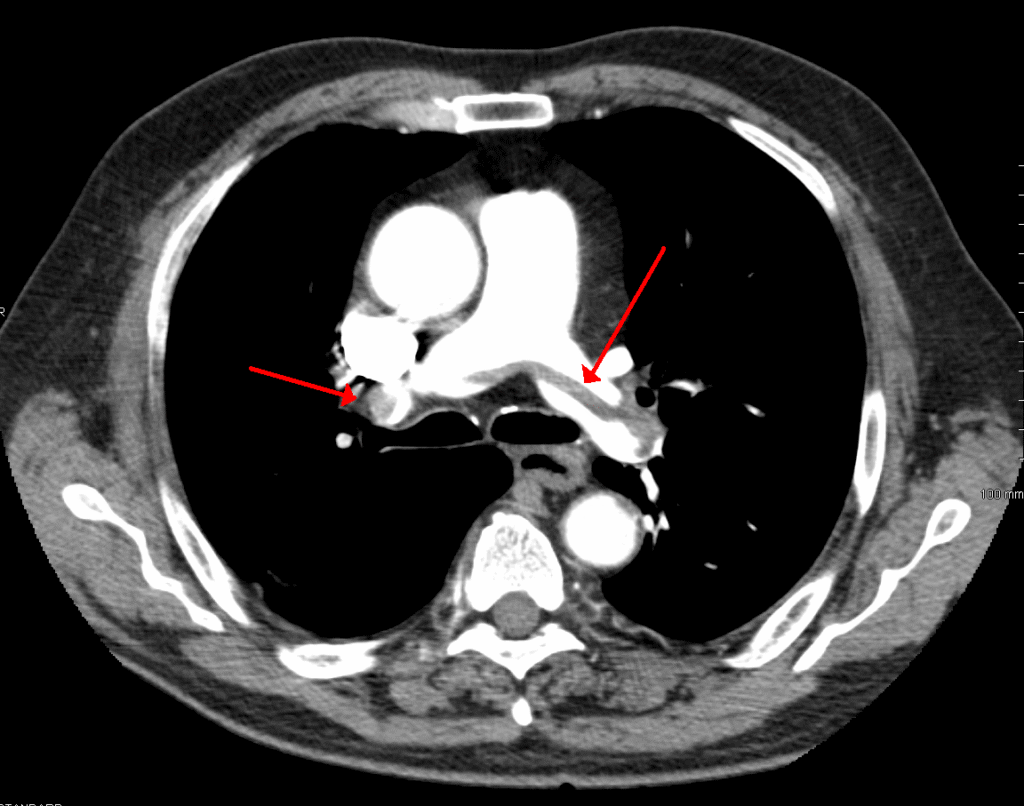
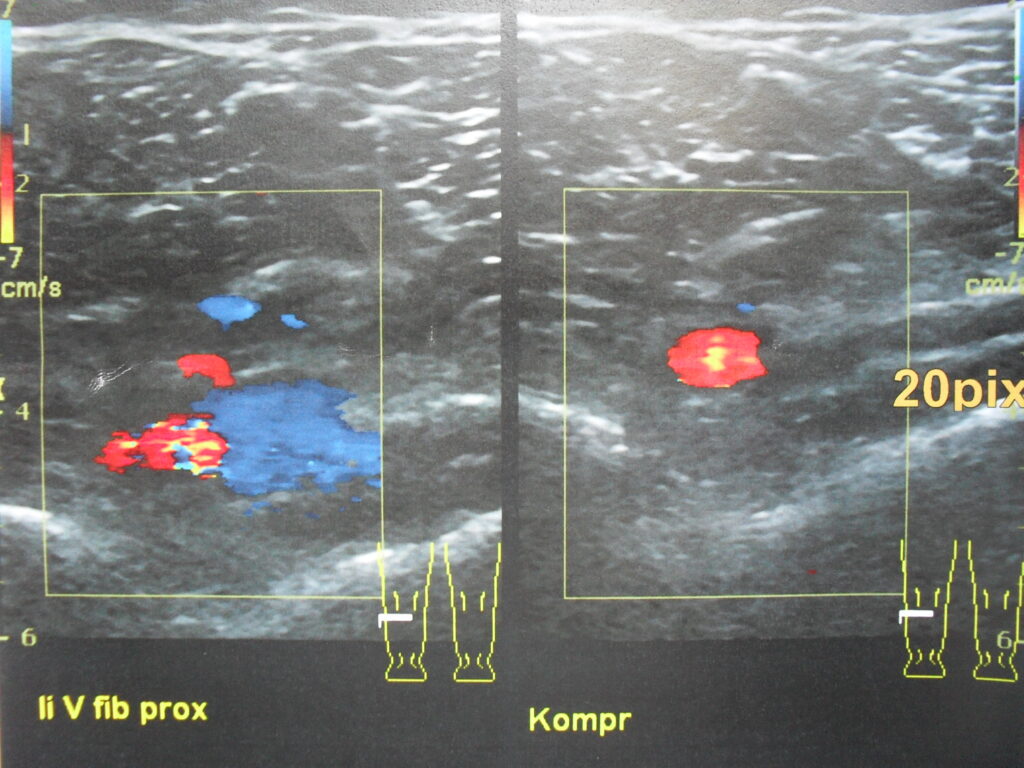
I underwent a chest x-ray (spiral CT scan), followed by an ultrasound. These revealed clots in both lungs and my left calf.
I spent the first night in intensive care, where I began anticoagulant therapy with heparin by infusion. The purpose of this was not to break the clots up, but to prevent them from getting larger and more clots forming. The following day, I moved to a general ward and was put on apixaban, an oral anticoagulant.
Anticoagulants
We call anticoagulants “blood thinners,” possibly because they’re known to increase the risk of bleeding. What they actually do is reduce the blood’s ability to clot.
Currently, oral anticoagulants are categorized as vitamin K antagonists and non-vitamin K antagonists.
This refers to vitamin K1 and not vitamin K2. This article goes into more detail.
Vitamin K Antagonists (VKAs)
Put very simply, VKAs disrupt the vitamin K cycle to disable vitamin K-reliant clotting factors. Consequently, vitamin K is the antidote, which is useful in the event of major bleeding, but inconvenient on a day-to-day basis; patients are subject to dietary restrictions, regular monitoring, and continuous dosage adjustments.
Warfarin is still the most well-known anticoagulant, but clinicians increasingly favor non-VKAs.
Non-Vitamin K Antagonists (Non-VKAs)
These are also known as novel oral anticoagulants (NOACs) and directly acting oral anticoagulants (DOACs).
Non-VKAs include apixaban, edoxaban, and rivaroxaban, which are collectively referred to as xabans. Because these inhibit the clotting factor Xa directly, there are no food interactions.
A further non-VKA is dabigatran, which inhibits the clotting factor IIa (thrombin).
A major disadvantage of non-VKAs was the absence of a reliable antidote, but the FDA eventually approved a drug called idarucizumab for dabigatran in 2015, and andexanet alfa for xabans in 2018.
Safety of Non-VKAs
With regard to bleeding incidents, studies on non-VKAs show that patients generally tolerate these well, with apixaban consistently ranking among the safest.
Nevertheless, individual responses can vary, and long-term safety still depends on personal health factors and clinical context. Therefore, be cautious and never take safety for granted.
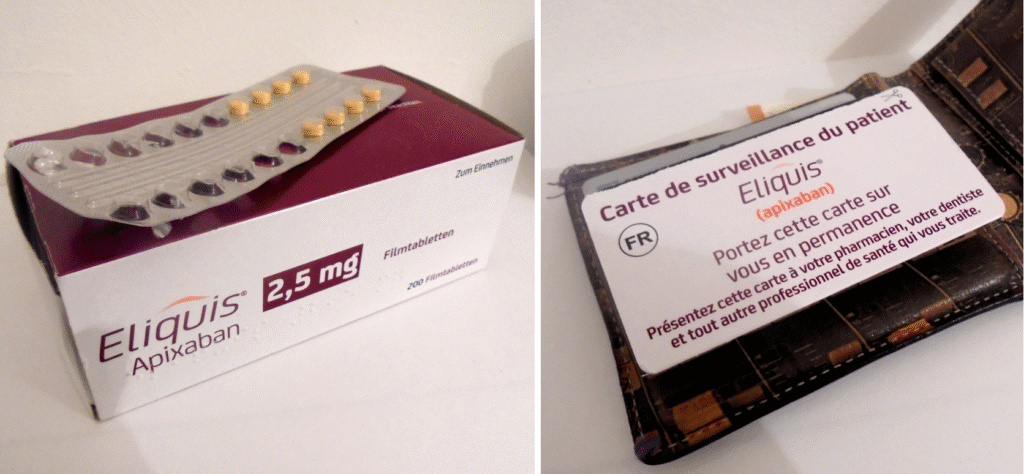
My Experience With Apixaban
Apixaban (trade name Eliquis) is the only oral anticoagulant I’ve used so far. The dosage for the first week was 20 mg daily, 10 mg for the next six months, then 5 mg as a lifelong preventive measure: tests concluded that I have a prothrombin gene mutation, which puts me at increased risk of developing further thrombosis.
Side Effects
Up to now I’ve experienced no significant side effects. I’ve occasionally observed traces of blood in my stool, but this is normal according to my doctor. However, what is normal for me may not be normal for you; it’s imperative that you tell your doctor of any irregularities, regardless of how minor or irrelevant these may seem.
Pausing Apixaban
Prior to undergoing a gastro- and colonoscopy, I stopped apixaban for 48 hours with no adverse reaction. This is necessary before any procedure where bleeding may occur, but always check with a doctor first.
How Using Apixaban Affects My Daily Life
On a day-to-day basis my life continues as before. But there are a few precautions to be aware of.
- Avoid activities that easily lead to injury, like contact sports. Until my dosage of apixaban was lowered to 5 mg per day, I also stopped wet shaving. I now cold shave. This constricts blood vessels, which can minimize bleeding in case of nicks and cuts.
- Due to the anticoagulant effect of non-steroidal anti-inflammatory drugs, like aspirin and ibuprofen, I use acetaminophen (paracetamol) unless otherwise advised by a doctor.
- Because alcohol is known as a “blood thinner,” consume no more than two standard drinks per day; I prefer to avoid it altogether.
- Because apixaban can lead to uncontrolled bleeding, I carry a patient alert card at all times in case of accident or emergency surgery (see photo above). These you’ll find in the product packaging in several languages, which is useful for travel.
Compression Socks and Stockings
As a preventive measure against post-thrombotic syndrome, a possible long-term condition resulting from DVT, it’s recommended to wear a compression sock or stocking for at least two years after diagnosis. By then, symptoms should have subsided, particularly discoloration and swelling.
Unfortunately, I did develop post-thrombotic-syndrome as a result of delayed treatment, and must therefore wear compression hosiery for life. My symptoms include varicose and spider veins of the foot and leg.
In this context, varicose veins form when blood reroutes from compromised veins deeper in the leg.. Doctors advise not to remove them.
Knee- or Thigh-Length?
If the thrombus and subsequent swelling are confined to the calf, you’ll probably be told to wear a knee-length sock. Because I experienced pain in my thigh, I wore a thigh-length stocking for the first three years, then knee-length.
How Compression Socks and Stockings Work
Compression socks and stockings use strong elastic to apply pressure around the leg, helping prevent blood from flowing backward. Treating DVT relies on graduated compression, whereby the stocking fits more tightly at the ankle than the calf and/or thigh.
Strengths
Strength is measured in mmHg (millimeters of mercury). My stocking, for example, measured 23–32 mmHg, meaning it was 32 around the ankle and 23 around the thigh. This is referred to as grade 2 strength, which is recommended for the treatment of DVT.
Sizing
A good fit is critical. This is achieved by measuring the narrowest part of the ankle, the broadest part of the calf, and the length from the floor to the knee. For thigh-length stockings, measure the length from the floor to the top of the inside leg, and add the broadest part of the thigh.
Caring for Compression Socks and Stockings
Body substances impair elasticity; therefore, wash daily using a mild, liquid detergent for delicate fabrics, and hang out to dry naturally. Never machine wash or tumble dry. This way, your socks or stockings will remain in relatively good condition until you need to replace them—usually after six months.
Putting On Compression Socks and Stockings
While I was in the hospital, a manufacturer’s representative fitted my first compression stocking. Unfortunately, the heel wasn’t properly aligned to my own heel, which caused a great deal of pain and left a welt. Before pulling the sock or stocking on, make sure the seam at the top lines up to the center of your heel exactly.
The Sigvaris website has an array of instructional videos showing how to put on various types of compression hosiery.
Extra tip: To prevent them from falling down, thigh-length stockings usually have a silicone grip band at the top. But it won’t work if you apply any kind of moisturizer or talc, and you may have to shave your thigh.
Exercises and Extra Tips
Do these three very simple exercises whenever you find yourself sitting for extended periods, especially when in a confined space:
- Stretch your leg out before you and whip your foot to and fro.
- Keeping it on the floor, rock your foot from heel to toe. You should notice some strain in the calf.
- Lift your foot from the floor, thus raising the knee and activating the thigh.
Repeat each exercise several times, at least every hour.
My doctor gave me the following tips:
- Before stepping out of the shower, run cold water over your calf. This causes the veins to contract and the blood to flow more forcefully.
- Raise the foot of your bed by about six inches to prevent the blood from flowing backward while you sleep.
This is a revised version of my original article “DVT and PE: Causes, Symptoms, Treatment, and Prophylaxis,” first published on Patient’s Lounge in 2019.
© 2025 J. Richardson
Related Posts
Disclaimer
The information provided by The Neat and Tidy Man (“we,” “us,” or “our”) on theneatandtidyman.com (the “site”) is for general informational purposes only. While we endeavor to keep the information up to date and correct, we make no representation or warranty of any kind, express or implied, regarding the completeness, accuracy, reliability, suitability, adequacy, validity, or availability of any information on the site. Under no circumstance shall we have any liability to you for any loss or damage of any kind incurred as a result of the use of the site or reliance on any information provided on the site. Your use of the site and your reliance on any information on the site is solely at your own risk.



